28 Mar 2018
A range of organisations, businesses, clubs, groups and communities across Scotland have already installed an Automated External Defibrillator. Many make them available to the general public and visible to emergency services: such Public Access Defibrillators (PADs) are key to strengthening community readiness to respond to an OHCA.
While RRG is working with partners to gather evidence on how PADs might best be used in Scotland, we are eager to offer advice to those thinking of placing a PAD in their community.
This guide, prepared by the OHCA Strategy Delivery Group, aims to outline key things that individuals and communities should consider before purchasing and installing a PAD.
Special thanks to John Fotheringham for his work in drafting the guide.
A link to the guide can be found here

07 Mar 2018
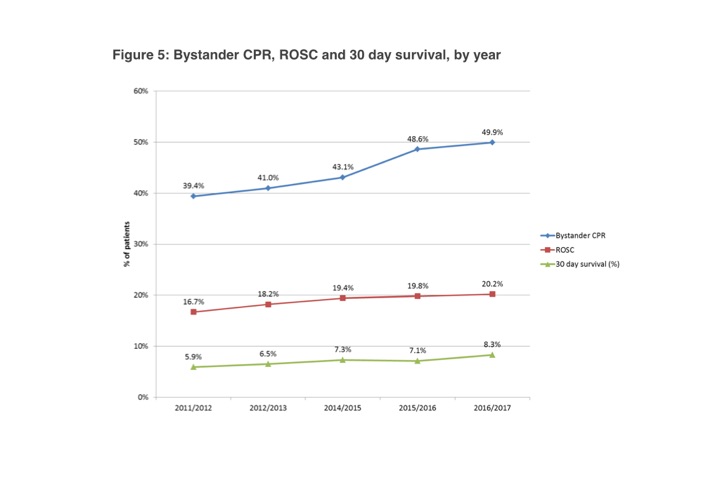
Half of the Scottish adult population do not feel confident administering CPR – and more than a fifth do not know when it is required, according to a collaborative study involving the RRG and the University of Stirling.
The study, which has been welcomed by the Scottish Government, is the first to examine the readiness and willingness of Scots to carry out cardiopulmonary resuscitation (CPR). Experts believe the work could help to explain why our survival rates from cardiac arrest are poor when compared to other countries.
Fiona Dobbie, a Research Fellow at the Institute of Social Marketing, part of the Faculty of Health Sciences and Sport, led the work, which also involved the Resuscitation Research Group at the University of Edinburgh and the Scottish Government.
“The findings of our study will help develop policy and future interventions to improve the rate of bystander CPR,” Ms Dobbie said. “From a policy perspective, there is a need for more tailored and targeted interventions to encourage CPR training, which has been linked with improving confidence in CPR. As confidence increases, so does the likelihood of providing emergency aid in an out-of-hospital cardiac arrest.
“Our findings suggest that priority groups are people who are not working, in a lower social grade and the elderly.”
In 2015, Scotland’s Strategy for Out-of-Hospital Cardiac Arrest was launched with the aim of equipping 500,000 people with CPR skills in a bid to save an additional 300 lives per year following an out-of-hospital cardiac arrest.
The new study, which informs the Strategy, comprised an Ipsos MORI survey, which canvassed 1,027 adults in Scotland.
Fifty per cent said they would not feel confident administering bystander CPR, with a further 21 per cent admitting that they would not know if it was required.
Twenty-two per cent would not be comfortable giving CPR, for fear of causing an injury to the victim, while 19 per cent would be reluctant due to their lack of skills. The same proportion would be put off by visible vomit or blood and 16 per cent by indications that the ill person is a drug user, the poll found.
The team found that confidence was affected by age, social grade and employment status; the older the person was, the less likely they were trained in CPR, show willingness to be trained, or feel confident to administer CPR. Fifty-eight per cent of 35 to 44 year olds said that they would like to be trained in CPR, compared to just 37 per cent of 55 to 64 year olds and 23 per cent of those aged 65 and over.
Respondents with professional, managerial and non-manual occupations were more likely to have been trained in CPR than those in manual, unskilled occupations and the long-term unemployed.
Dr Gareth Clegg, a Senior Clinical Lecturer at the University of Edinburgh, an Honorary Consultant in Emergency Medicine at Edinburgh Royal Infirmary, and an Associate Medical Director, of the Scottish Ambulance Service, co-authored the paper.
He said: “Survival from cardiac arrest in Scotland is a poor relative to the best performing centres in the world. One of the most important determinants of survival is bystander CPR, which more than doubles chances of survival.
“We already know that people in the most deprived areas in Scotland are much more likely to have a cardiac arrest, at a younger age, and less likely to survive than those in affluent areas.
“This work is important because it suggests that those living in communities which are most likely to need CPR are least ready to carry it out.”
Dr Clegg added: “Using the findings from this research, we hope to develop ways to teach hundreds of thousands of people in Scotland how to perform CPR – and save hundreds more lives each year.”
Minister for Public Health Aileen Campbell said: “That half of adults in Scotland in this survey were already confident giving CPR gives us a firm foundation to build on, and to date more than 200,000 people across the country have learned CPR since 2015.
“This is great progress towards our 500,000 target by 2020 and a testimony to the work put in by our Save A Life For Scotland partnership, who have brought these lifesaving skills to more people across the country.
“Any CPR is better than no CPR and we know it’s the main way we can increase survival after Out of Hospital Cardiac Arrest.”
The study, Attitudes towards bystander cardiopulmonary resuscitation: results from a cross-sectional general population survey, was commissioned by the Resuscitation Research Group at the University of Edinburgh and is published in PLOS ONE.
29 Nov 2017
On Friday 17th November, the Resuscitation Research Group held the first of the new series of Edinburgh Conversations.
The theme of the Conversation was the ‘Prior Hypothesis’. Experts met to discuss the effects of capillary pore size, pulse waves and osmotic pressure on fluid exchange, with a view to thinking about implications for future research and clinical practice.
It was the opportunity to release the initials results of the Prior Study, which was led by Allan MacRaild, Senior Research Nurse in EMERGE.
Dr Frank Prior was joined by Dr Colin Robertson, Dr Gordon Drummond, Mr Peter Jones, Mr Allan MacRaild and Dr Gareth Clegg. Discussions from the event will help strengthen the hypothesis and uncover unexplored areas.

The Prior Hypothesis – an update to the Starling Hypothesis – offers a new model of fluid balance and exchange.
Fluid balance and exchange are driven by the balance of two opposing pressures, the blood pressure which filters fluid out of the capillary and the osmotic pressure which draws fluid back into the plasma. Our physico chemical studies show that osmotic pressure is dependent on both concentration and membrane pore size. Increasing the concentration increases the osmotic pressure. Increasing pore size causes a fall in osmotic pressure. These three major factors determine osmosis. A knowledge of two of them should enable the third to be calculated. To test this concept we have measured membrane osmotic pressures (MOPx) and calculated capillary pore sizes during lying and standing, temperature stress, arm occlusion and simulated dives in human volunteers. We have also calculated pore size during anaesthetic induction, throughout Major GI surgery, and during pulsatile and non pulsatile cardiac bypass.
These results are included in our book entitled The Prior Hypothesis, which is in the final proof reading phase.